What is PCOS?
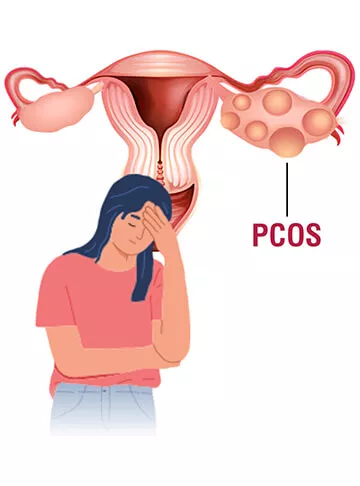
Polycystic Ovary Syndrome, commonly known as PCOS, is a prevalent hormonal disorder that affects people assigned female at birth. PCOS is a medical condition characterized by an imbalance of hormones in individuals with ovaries. It is a complex condition with various manifestations and impacts on reproductive, metabolic, and overall health. One of the key features of PCOS is the presence of small, fluid-filled sacs or cysts in the ovaries, which can interfere with normal ovulation. This disruption in the menstrual cycle can lead to a range of symptoms and complications.
By definition, PCOS (Polycystic Ovary Syndrome) is a hormonal condition that interferes with the normal functioning of the ovaries. That is, it leads to overproduction of androgen hormones from the ovaries, causing irregular ovulation. As a result of this irregularity, many women experience immature follicular cysts and irregular periods, either early or delayed.
The condition can be even more frustrating for women trying to conceive, as irregular periods make tracking their menstrual cycle a challenge. It is a chronic condition, but that should not make you think that it is not manageable. With early diagnosis and available management options, women can significantly keep their hormones in check, maintain menstrual regularity, and improve overall reproductive well-being.
What are the Types of PCOS?
PCOS is not the same for every woman; that is, it can be present in different types, classified based on its triggers and hormonal imbalance. These PCOS types greatly determine the treatment approach and symptoms:
- Insulin-resistant PCOS: It is a trigger-based form of PCOS characterised by reduced insulin sensitivity.
- Inflammatory PCOS: This type is generally a result of long-term low-grade inflammation.
- Adrenal PCOS: Adrenal is a stress hormone, and overproduction of this hormone can lead to elevated androgens and ultimately PCOS.
What are the Causes of PCOS?
Although the exact cause of PCOS is not fully understood, several different key factors are known to play a major role in disrupting the hormonal balance of the body. The following are the estimated causes of PCOS that work together to result in the trademark symptoms of the condition:
- Hormonal Imbalance: An increased production of the androgens, which are normally present in small amounts in women, negatively impacts the normal ovulation and menstrual regularity.
- Insulin Resistance: The body knows how to use its sugar, but when it fails to do so, excessive androgen production finds a way.
- Genetic Factors: A family history of risk factors for PCOS increases the likelihood of developing the condition.
What are the Symptoms of PCOS?
As mentioned earlier, symptoms of PCOS vary based on the type of the condition. However, there are some symptoms that remain constant for each type and every woman facing PCOS, which may include:
- Unpredictable and irregular periods, either delayed, early or missed.
- Acne and oily skin
- Excessive growth of facial and body hair
- Thinning of hair and scalp
- Irregular weight, either difficulty gaining or losing it.
- Dark skin patches
- Difficulty in conceiving due to unpredictable ovulation.
- Extra skin (skin tags) protruding out of the armpits.
- Cyst formation due to follicle accumulation as a result of irregular periods.
What are the Risks and Complications of PCOS?
PCOS is a long-term or chronic condition that requires proper, early management. However, if left untreated, the condition can complicate and threaten multiple bodily functions. Some of the most common ones may include:
- Infertility due to irregular and absent ovulation as a result of untreated PCOS.
- Type 2 diabetes and prediabetes, when the cause of PCOS is insulin resistance.
- Obesity and metabolic syndromes make it harder for the body to maintain hormonal balance.
- High Blood Pressure
- High fat and cholesterol levels.
- An increased risk of cancer.
- Inability to sleep or sleep apnea
- Heart and other vascular issues over time.
How is PCOS Diagnosed?
As the statistics say themselves, almost 70% of the women with PCOS remain undiagnosed until the condition becomes more complicated. Therefore, diagnosis is the first line of defence you can provide to your body, which is generally done with a combination of medical and physiological tests, such as:
Clinic Assessment:
The diagnosis generally begins with your first consultation with your doctor, who will review your complete family, medical, and menstrual history. For instance, your doctor may assess things like:
- The regularity of your menstrual cycle, whether it is regular, irregular, or completely gone, meaning absent.
- Symptoms such as acne, excessive hair growth, weight gain, and signs of insulin resistance.
- Whether the condition runs in your family or not.
Blood Tests:
The next step is hormonal profile tests that identify and confirm irregularities in certain reproductive hormones. The hormones generally checked during this blood test are:
- Luteinizing Hormone (LH)
- Follicle-Stimulating Hormone (FSH)
- Total and Free Testosterone
- Insulin and Fasting Glucose Levels
- Anti-Müllerian Hormone (AMH)
Pelvic Ultrasound:
To look into the uterine structural, such as the ovaries and fallopian tubes, a transvaginal or abdominal ultrasound is used, with some key findings as follows in case of PCOS:
- Follicle Count: A follicle count of ≥12–20 per ovary is often a sign of ovarian follicles seen in PCOS.
- Ovarian Volume: An enlarged ovary may be observed due to the accumulation of follicles in the case of PCOS.
Note that follicle accumulation and appearance are not trademark only for PCOS; rather, they are common signs for various other uterine issues. Therefore, these ultrasounds, along with the interpretation of symptoms and hormone levels, are important to distinguish PCOS from other uterine issues.
Rotterdam Criteria:
The internationally accepted guideline to accurately diagnose, two of these three conditions must be satisfied to be classified as the confirmatory proof of PCOS:
- Irregular or absent ovulation
- High androgen levels are found in clinical and biochemical blood tests.
- Polycystic ovaries are found on the ultrasound.
Identifying PCOS early on becomes even more important when we understand the complications it may cause over time, as mentioned above. It allows management strategies to take their time to improve overall reproductive and uterine health.
How is PCOS Treated?
The treatment for PCOS generally depends upon the woman’s needs, whether she wants to manage or improve fertility. Since the symptoms and types may differ for every woman, a one-size-fits-all approach can not work every time. Therefore, a treatment plan is designed with respect to tackle the specific needs of a patient, such as:
Non-Fertility Treatment:
- Lifestyle Changes (Diet and Exercise): Lifestyle management is one of the first non-fertility treatments for PCOS. This includes:
- Taking a low-GI and balanced diet to control insulin in the body.
- Regular light exercise to improve metabolism, support BMI, and regain normal cycles.
- Hormonal Birth Control: Birth control pills or the contraceptive can also help manage PCOS; however, the option is only beneficial for women not trying to conceive. Here’s how these pills can help:
- Realign the menstrual cycles
- Reduce acne
- Control excess facial and body hair growth.
- Balance overproduction of androgen hormones.
- Metformin for Insulin Resistance: Metformin is a powerful medicine, generally used to manage diabetes. Therefore, in case of PCOS caused by insulin resistance, it can also help by:
- Controlling insulin and androgen levels in the blood.
- Regulate ovulation
- Support weight management
- Reduce the risk of type 2 diabetes.
Fertility–Focused Treatment:
- Ovulation Stimulation: Women considering conceiving can go for ovulation-stimulating drugs, as prescribed by the doctor. These medications are used to induce ovulation to increase the chances of natural conception.
- Laparoscopic Ovarian Drilling (LOD): It is a minimally invasive surgery, generally recommended when oral medications fail to work. It helps to enhance fertility by lowering androgen levels and restoring regular ovulation.
- In Vitro Fertilisation (IVF): For women expecting to conceive and have PCOS, IVF becomes the best option when other treatments fail. It involves stimulating the ovaries and fertilising in a controlled environment.
Indira IVF can offer a personalised treatment plan for every woman as per their hormonal profile, fertility goals, and medical history to optimise the best results out of it.
When Should You See a Doctor?
Early evaluation and diagnosis are the best treatment for PCOS, because timely treatment is the key to long-term healthy reproductive health. Therefore, to make things work in your favour, always keep an eye on the following symptoms of PCOS and seek immediate medical help if you catch any:
- Irregular or missed periods
- Excessive growth of facial or body hair
- Severe acne out of nowhere
- Unexpected weight changes
It is also crucial to seek medical help if you are unsuccessful for several months in conceiving.
Frequently Asked Questions (FAQs)
Is PCOS curable?
While PCOS cannot be completely cured, it is possible to manage the condition through dietary and activity modifications and with the use of medical therapies.
Can PCOS cause infertility?
Many women with PCOS do get pregnant through the treatment and assistance. However, PCOS often disrupts ovulatory function, making it difficult for women to conceive.
Do women with PCOS have a higher risk of developing diabetes?
The presence of insulin resistance associated with PCOS is a major risk factor for developing type 2 diabetes later in life.
Can PCOS be prevented?
Maintaining a healthy lifestyle, eating the right foods, staying active, and managing weight can help manage PCOS.
Is it possible to reverse PCOS through extreme weight loss and improved lifestyle habits?
Losing a small amount of weight may restore normal hormone function, regular ovulation and improve regular menstrual cycles for women suffering from PCOS.
Does PCOS affect in vitro fertilisation (IVF) success?
The success rates of IVF for women suffering from PCOS may increase when the stimulated cycle is carefully controlled.
What is the difference between PCOD and PCOS?
In PCOD, there are multiple ovarian cysts and milder, less noticeable symptoms. On the other hand, PCOS is a more severe form of a hormonal condition that has more extensive metabolic and fertility implications.
Who is at risk for developing PCOS?
PCOS may affect women of reproductive age; however, women who have a family history of hormonal or metabolic problems are at the most significant risk.
What are some lifestyle changes you can make to help with PCOS?
Exercise regularly, follow a well-balanced, low glycemic index (GI) diet, maintain a healthy weight, get sufficient sleep, reduce stress, etc., can help significantly manage PCOS.
Pregnancy Calculator Tools for Confident and Stress-Free Pregnancy Planning
Get quick understanding of your fertility cycle and accordingly make a schedule to track it
Get a free consultation!