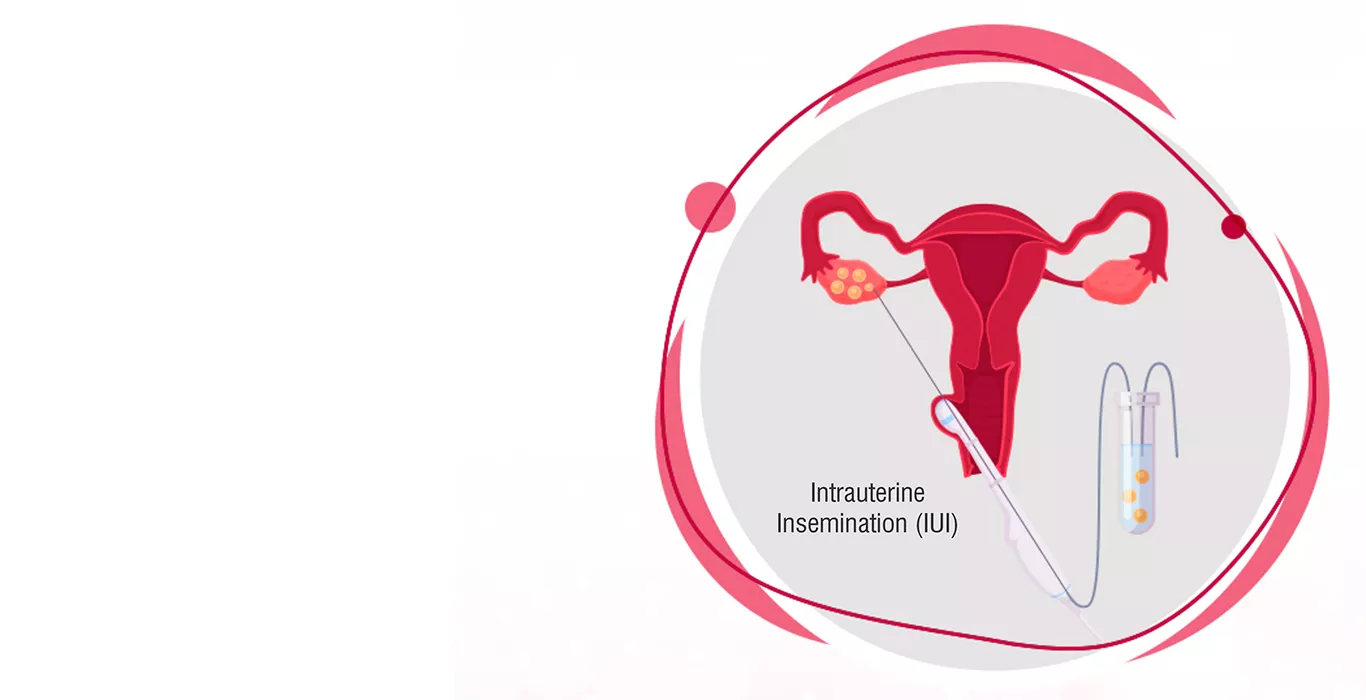
What is IUI (Intrauterine insemination)?
IUI, or Intrauterine Insemination, is a popular fertility treatment where healthy sperm cells are injected into a woman's uterus to facilitate fertilisation. IUI is a simple and non-invasive procedure that is commonly used in cases where couples experience difficulty in conceiving.
Intrauterine means “inside the uterus” thus, intrauterine insemination is the process wherein the best quality sperms are introduced into the uterus to fertilise the egg. The objective here is to bring the sperms as close to the egg as possible.
Whether to perform IUI or not is decided by several factors, as per the doctor's recommendation and the patient's individual situation.
Steps involved in IUI Treatment
The process of IUI involves several steps, which are as follows:
1.Ovarian stimulation: The woman is given fertility medication to stimulate ovulation, which helps to increase the number of eggs that are released during ovulation.
2.Monitoring of ovulation: The woman's ovulation is monitored through ultrasound and blood tests to determine the optimal time for the IUI treatment.
3.Sperm preparation: The sperm sample is prepared through a process called sperm wash, which involves removing dead or slow-moving sperm cells and concentrating the quality sperm.
4.Insemination: The healthy sperm is injected into the woman's uterus through a small catheter.
Post-procedure care: After the procedure, the woman may be advised to rest for a short period and avoid heavy lifting or strenuous exercise.
IUI is a relatively low-cost fertility treatment, which makes it a popular choice for many couples. It is considered less invasive than other fertility treatments, such as IVF, which is a more complicated and expensive process.
Success Rate of IUI
The success rate of IUI fluctuates depending on many factors, such as the age of the woman, the reason for infertility and the quality of the sperm injected.
The success rate of IUI is highest for couples experiencing infertility due to issues with the male sperm. In these cases, the sperm from the male partner can be washed and concentrated before being injected into the uterus, which can improve the chances of successful fertilisation. However, the success rate of IUI is lower for couples experiencing infertility due to issues with the woman's reproductive system.
Overall, the success rate of IUI ranges from 10-20% per cycle, with up to 80% of couples achieving pregnancy after six cycles of IUI. However, the success rate of IUI decreases as the woman's age increases, with a success rate of only 4% for women over the age of 40.
Advantages of IUI
- Increased chance of pregnancy: IUI improves the chance of fertilisation because it places sperm directly in the uterus, close to the fallopian tubes where fertilisation occurs.
- Lower cost compared to other fertility treatments: IUI is less expensive than in vitro fertilization (IVF), making it a more affordable option for couples who are struggling with infertility.
- Minimal discomfort: The IUI procedure is relatively simple and does not require general anaesthesia, which means it is generally less painful and more comfortable than other fertility treatments.
- No need for medication to stimulate ovulation: In some cases, IUI can be performed without the use of fertility medication to stimulate ovulation, which can reduce the risk of complications and side effects associated with fertility drugs.
- Can be used in combination with other treatments: IUI can be combined with other fertility treatments, such as ovulation induction or intracytoplasmic sperm injection (ICSI), to further improve the chances of success.
- Fewer risks of multiple pregnancies: IUI has a lower risk of multiple pregnancies than other fertility treatments, such as IVF, which can increase the risk of complications for both the mother and the babies.
- Helpful for male fertility issues: IUI can be used to treat some male fertility issues, such as low sperm count or poor sperm motility, by placing a higher concentration of healthy sperm closer to the egg.
Disadvantages of IUI Treatment
- Lower success rates: Compared to other fertility treatments such as IVF, IUI has lower success rates, especially for couples with certain fertility issues like blocked fallopian tubes, PCOS, etc.
- Increased risk of multiple pregnancies: IUI can increase the likelihood of having twins, triplets, or more, which can increase the risk of complications during pregnancy and childbirth.
- Potential for infection: Inserting a catheter into the uterus during the IUI procedure can increase the risk of infection, particularly if there is already an existing infection in the reproductive system.
- Limited benefits: IUI may not be effective for couples with certain types of infertility, such as severe male factor infertility or tubal blockages, which is where IVF treatment works as a great option.
Intrauterine Insemination is a safe and effective fertility method that can be a viable option for couples who are experiencing difficulty conceiving. While it may not be suitable for everyone, it has several advantages over other fertility treatments, including its simplicity, affordability, and natural approach.
Pregnancy Calculator Tools for Confident and Stress-Free Pregnancy Planning
Get quick understanding of your fertility cycle and accordingly make a schedule to track it
Get a free consultation!